Fibroids
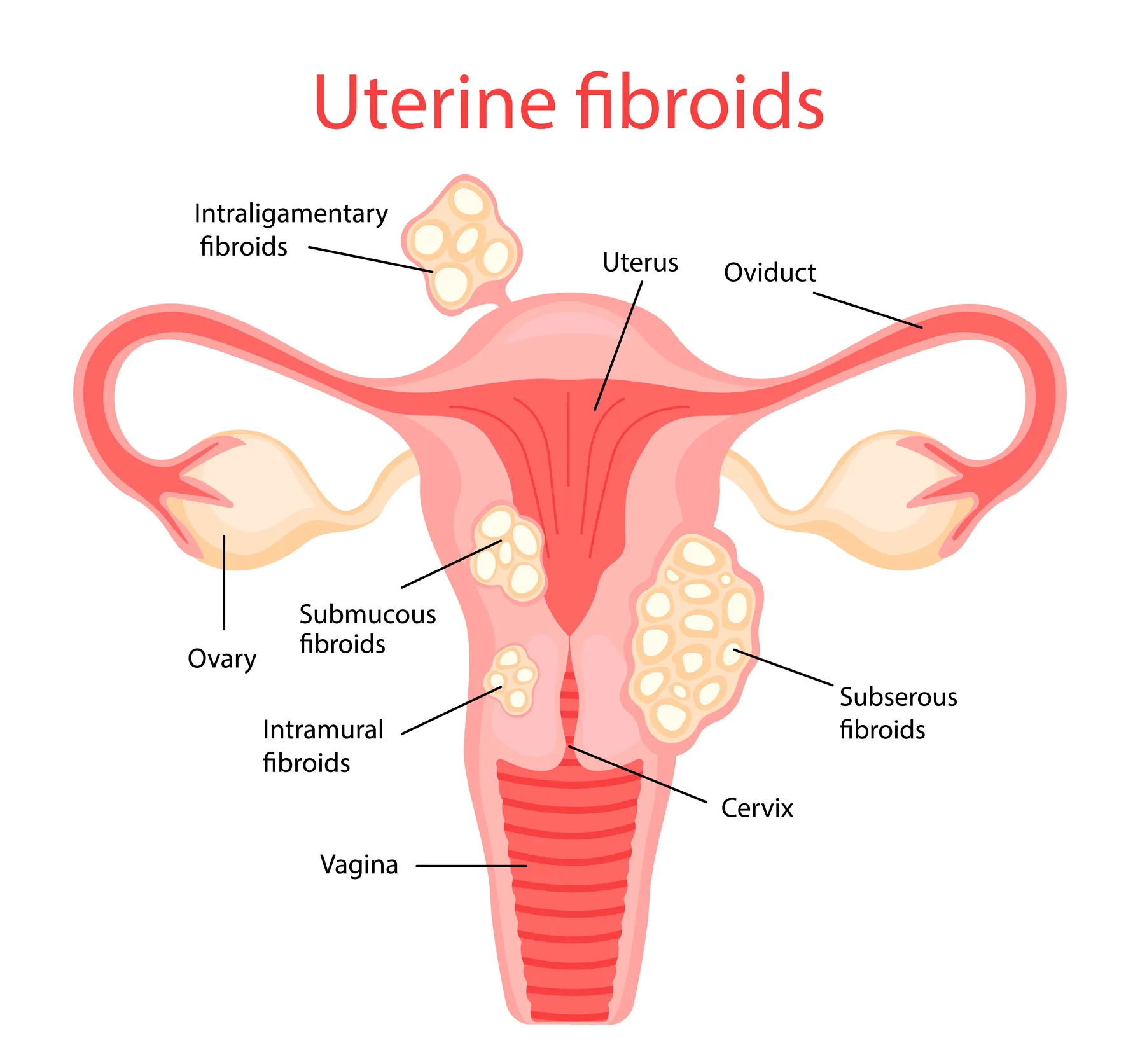
Fibroids, also known as uterine leiomyomas, are noncancerous growths that develop in the uterus, commonly during a woman's childbearing years. These growths can vary in size, number, and location within the uterus.
Symptoms of Fibroids
While many women with fibroids may not experience symptoms, others may experience a range of issues, including:
• Heavy menstrual bleeding
• Pelvic pressure or painFrequent urination
• Constipation
• Backache
Treatment Options for Fibroids
The treatment for fibroids largely depends on factors such as the size and location of the fibroids, the severity of symptoms, and whether the woman plans to have children in the future. Below are the common treatment options:
1. Watchful Waiting
For small fibroids that do not cause symptoms, doctors may recommend regular monitoring without any immediate intervention. This approach is typically adopted if the fibroids are asymptomatic.
2. Medications
If symptoms such as heavy bleeding or pelvic pain occur, hormonal medications or other drugs may be prescribed to manage and alleviate these issues. These medications can help reduce the severity of symptoms but do not eliminate the fibroids themselves.
3. Minimally Invasive Procedures
For women who are experiencing symptoms but wish to preserve fertility, there are several minimally invasive options:
• Uterine Artery Embolization: A procedure that blocks blood flow to the fibroids, causing them to shrink.
• Myomectomy: A surgical procedure that removes the fibroids while preserving the uterus, ideal for women who wish to maintain their fertility.
• MRI-Guided Focused Ultrasound Surgery (FUS): A non-invasive procedure that uses high-frequency ultrasound waves to destroy fibroids.
4. Hysterectomy
In cases where symptoms are severe and fertility is not a concern, a hysterectomy — the surgical removal of the uterus — may be recommended as a permanent solution.
Consult Your Healthcare Provider
It's crucial to consult with a healthcare provider to receive an accurate diagnosis and a personalized treatment plan based on your specific needs and preferences. Each woman's situation is unique, and a tailored approach will ensure the best possible outcome.
 Contact Us
Contact UsEndometriosis
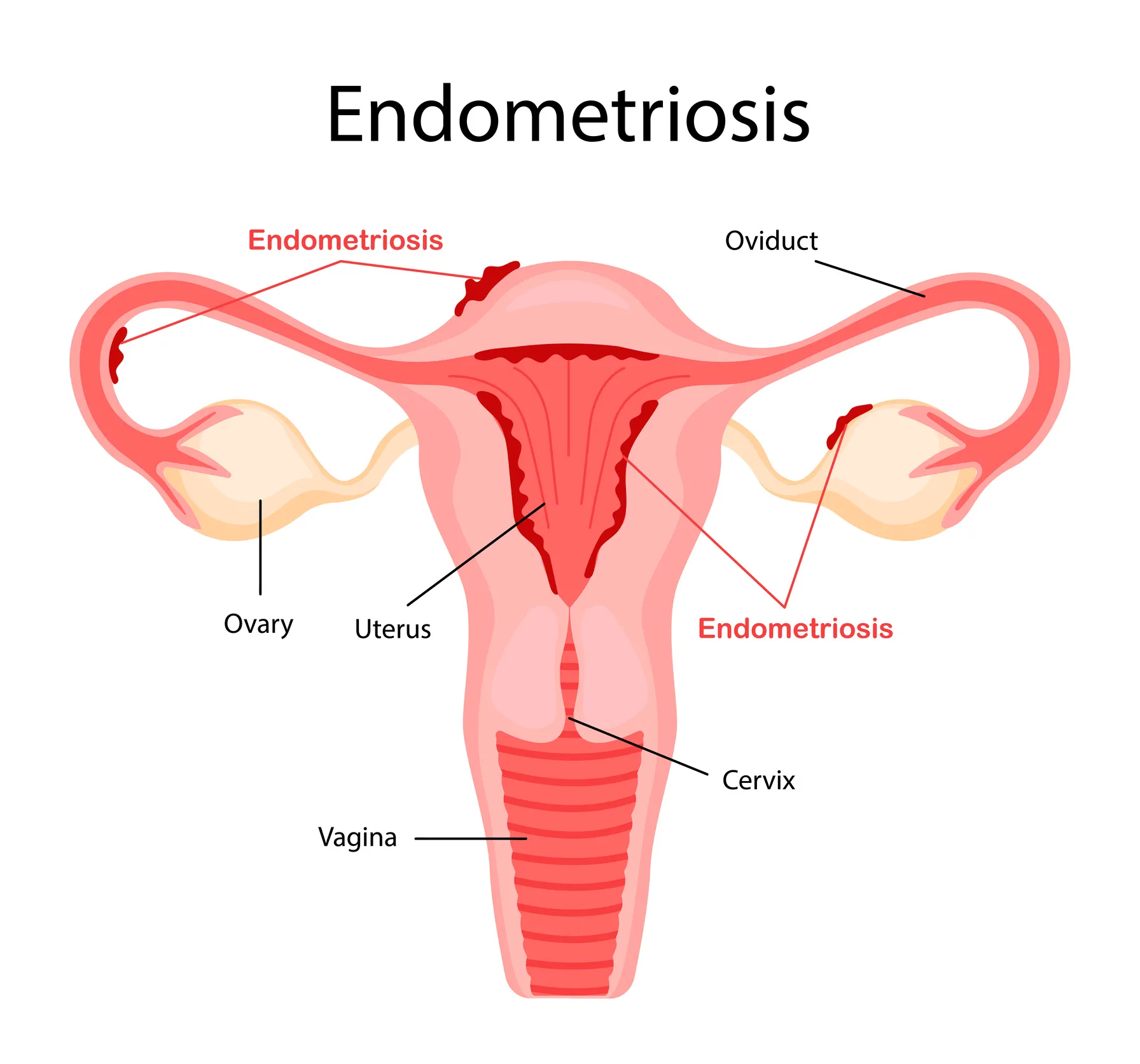
Endometriosis is a chronic condition in which tissue similar to the lining of the uterus (endometrium) grows outside the uterus, typically on the ovaries, fallopian tubes, and the tissues lining the pelvis. This misplaced tissue responds to menstrual cycle hormones, leading to inflammation, pain, and the formation of scar tissue (adhesions).
Common Symptoms of Endometriosis
The symptoms of endometriosis can vary in severity and may include:
• Pelvic pain, which often worsens during menstruation
• Painful periods
• Pain during or after intercourseInfertility
• Gastrointestinal symptoms, such as diarrhea, constipation, or bloating
• Bleeding in stools, severe dyschezia (painful defecation), or blood in urination during menstruation
Treatment Options for Endometriosis
While there is no cure for endometriosis, treatment focuses on managing symptoms and improving quality of life. Common treatment options include:
1. Pain Medication
Over-the-counter or prescription pain relievers, such as NSAIDs, can help alleviate discomfort and manage pain associated with endometriosis.
2. Hormonal Therapy
Hormonal medications, including birth control pills, hormonal IUDs, or other forms of hormonal therapy, can help regulate the menstrual cycle, reduce symptoms, and slow the growth of endometrial tissue.
3. Surgery
In more severe cases, laparoscopic surgery can be used to remove endometrial implants, scar tissue, and adhesions. If the condition is advanced, a hysterectomy (removal of the uterus) may be recommended.
4. Fertility Treatment
For individuals facing infertility due to endometriosis, fertility treatments such as in vitro fertilization (IVF) may be considered to increase the chances of conception.
Consult Your Healthcare Provider
If you are experiencing symptoms of endometriosis, it's crucial to consult a healthcare provider who is experienced in managing the condition. Early diagnosis and appropriate treatment can help improve both quality of life and fertility outcomes for individuals affected by endometriosis.
 Contact Us
Contact UsGynaecologic Cancer
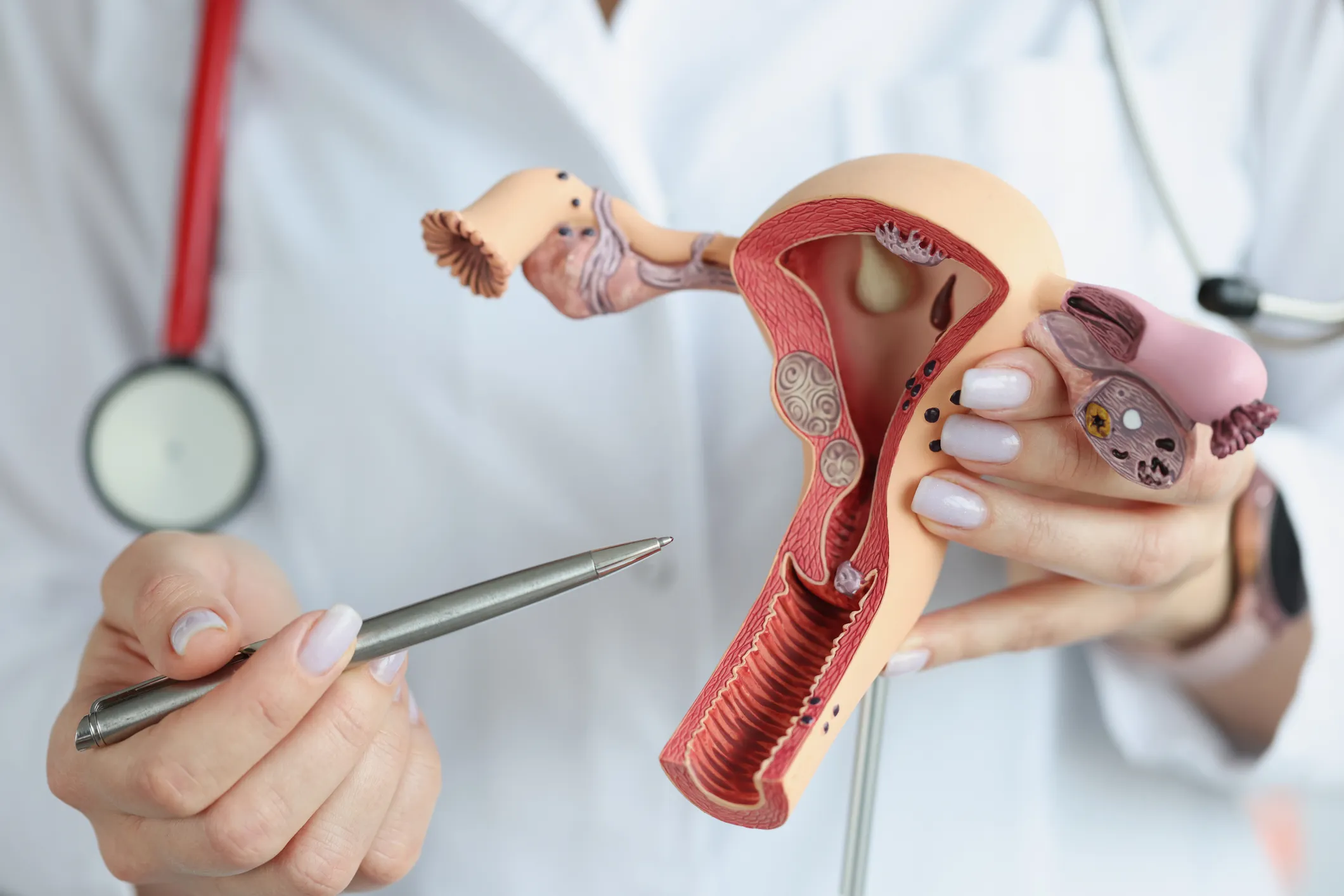
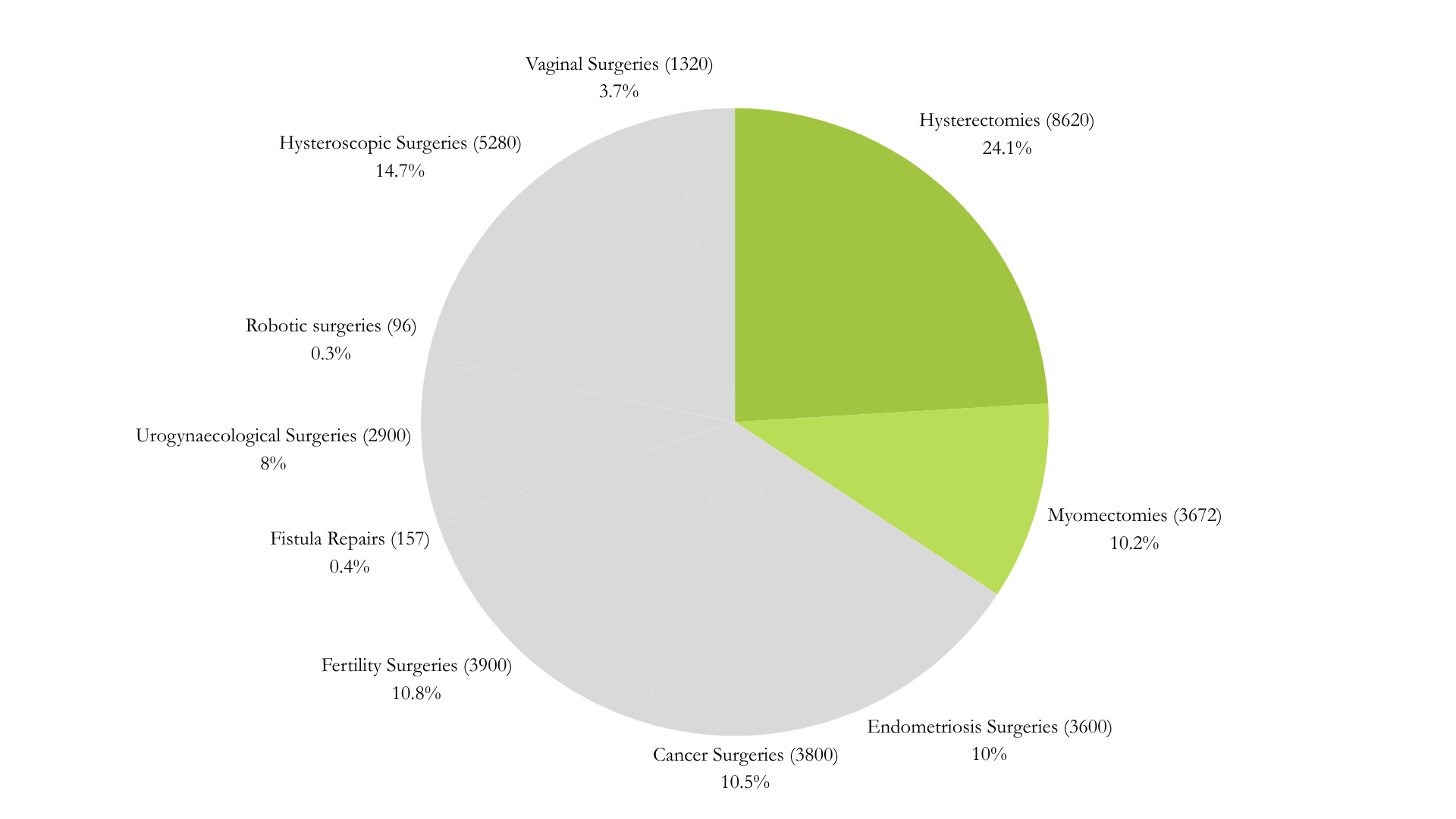
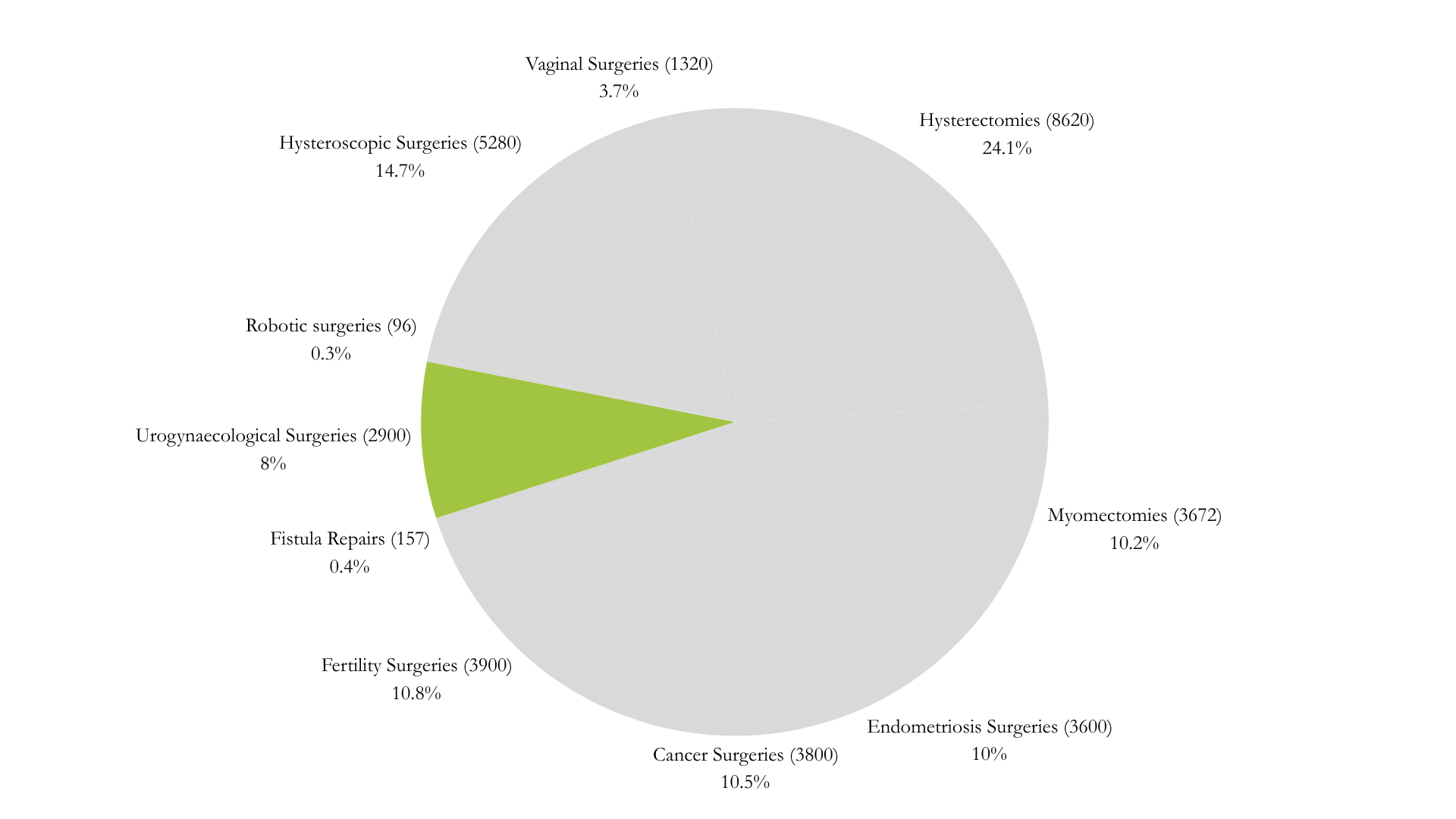
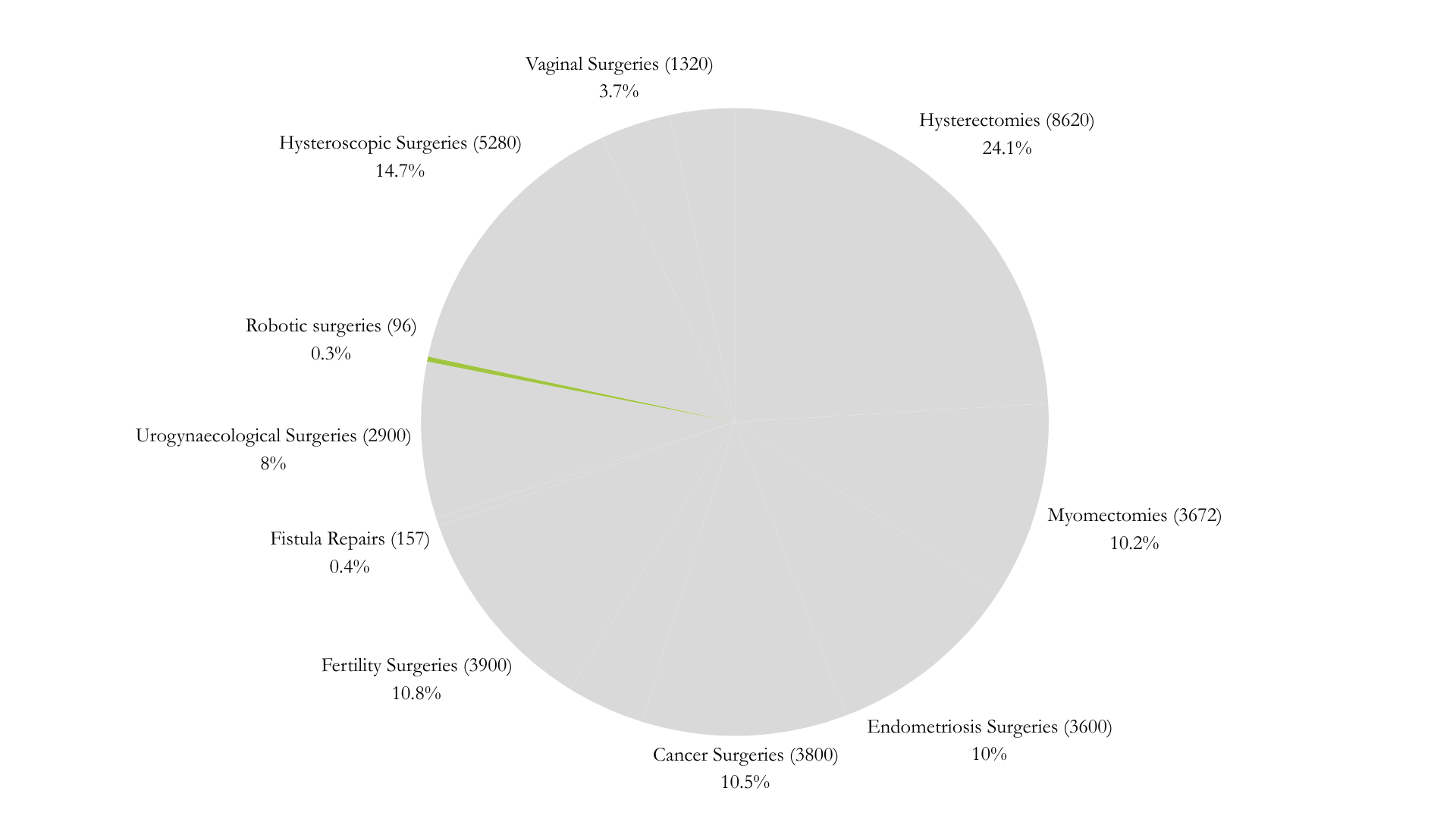
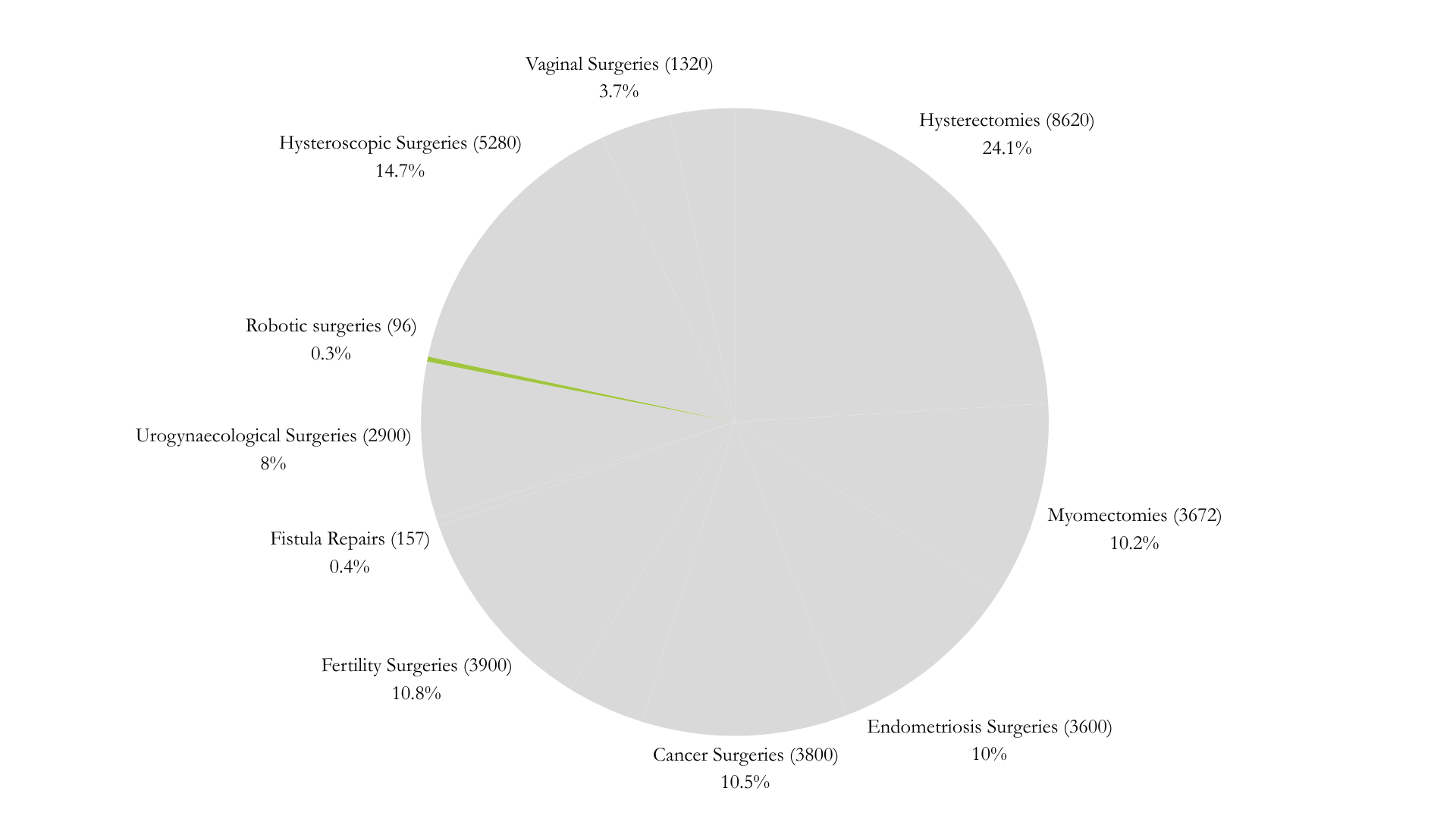
At Healthy Women, we are a pioneering center dedicated to providing advanced solutions for cancer treatment. With 19 years of experience, we specialize in offering radical surgical solutions using Laparoscopy and Robotics. Our expertise allows us to carefully select cases and provide optimal treatment options for each patient.
Our Achievements and Approach
We have successfully performed over 200-300 surgeries annually, maintaining a highly satisfactory recurrence-free rate and an extended disease-free survival duration. This success is a testament to our commitment to excellence and patient care.
At Healthy Women, we prioritize compassionate care. Our empathic approach, combined with our hands-on support for both patients and their families, ensures a holistic treatment experience that fosters trust and satisfaction. We believe in not only treating the disease but also providing emotional and psychological support, guiding our patients throughout their entire journey.
 Contact Us
Contact UsCosmetic Gynaecology

Female Sexual Medicine and Cosmetic Gynaecology are specialized fields that focus on improving sexual health, addressing intimate concerns, and enhancing the aesthetic aspects of the female genital area. These services offer a holistic approach to both physical and emotional well-being, empowering women to achieve greater satisfaction and confidence. Below is a detailed overview of the key services offered:
Labial Reduction (Labiaplasty): Surgical procedures to reduce or reshape the labia minora or majora, addressing both aesthetic and functional concerns.
Vaginal Tightening (Vaginoplasty): Surgical and non-surgical methods to enhance vaginal tone and reduce laxity, often used to address post-childbirth changes or age-related shifts.
Clitoral Hood Reduction: Surgical procedures to remove excess tissue around the clitoris, offering both aesthetic and functional improvements.
Laser Vaginal Rejuvenation: Non-invasive laser treatments designed to tighten and tone the vaginal area, improving sexual satisfaction and overall comfort.
Comprehensive Evaluation and Counseling
Personalized consultations are offered to address concerns related to sexual health, body image, and cosmetic goals. Psychological support and counseling services are available to help women address emotional or psychological factors affecting sexual well-being and body confidence.
Advanced Treatment Options
Cutting-edge technologies, such as lasers for rejuvenation and enhancement procedures, offer minimally invasive alternatives with reduced recovery time.
Infertility
At Healthy Women, we offer a wide range of solutions designed to help you achieve your dream of becoming a parent. Our holistic approach focuses on diagnosing and treating fertility issues systematically to support you through every step of the journey. Here are the key services we provide:
Diagnostic Testing
We conduct thorough assessments to identify the underlying causes of infertility, ensuring a tailored treatment plan that addresses your specific needs.
Medication
We offer medications to regulate ovulation and enhance sperm production, optimizing your chances of conception.
Assisted Reproductive Technologies (ART)
• Intrauterine Insemination (IUI): Sperm is placed directly into the uterus during ovulation to increase the chances of fertilization.
• In Vitro Fertilization (IVF): Eggs and sperm are combined outside the body and implanted into the uterus for a higher success rate in conception.
Surgical Interventions
We offer minimally invasive laparoscopic, hysteroscopic, and robotic surgeries to address anatomical issues affecting fertility, helping to create the optimal conditions for conception.
Lifestyle Modifications
We provide expert advice on diet, exercise, and lifestyle habits that can improve your fertility and support a healthy pregnancy.
Emotional Support
Fertility treatments can be an emotional journey. We offer counseling and support groups to help you navigate the emotional challenges and stay positive throughout the process.
Alternative Therapies
We integrate alternative therapies such as acupuncture and herbal supplements as part of a holistic approach to enhance fertility and well-being.
 Contact Us
Contact UsFistula repairs

Gynaecological fistulas are abnormal connections or passages that form between the vagina and nearby organs or tissues. These conditions can lead to significant health complications, requiring timely intervention and management. Below is an overview of the types, causes, symptoms, and treatment options for gynaecological fistulas:
Types of Gynaecological Fistulas
• Vesicovaginal Fistula (VVF): This condition involves an abnormal tract between the bladder and the vagina, leading to continuous urinary leakage into the vaginal vault. It is one of the most common types of gynaecological fistulas.
• Rectovaginal Fistula (RVF): This occurs when there is an abnormal connection between the rectum and the vagina, causing stool or gas to pass through the vaginal opening.
• Urethrovaginal Fistula (UVF): A less common condition where there is an abnormal connection between the urethra and the vagina, resulting in urinary leakage.
• Ureterovaginal Fistula (UPF): This is an abnormal connection between the ureters and the vagina, leading to continuous urine leakage through the vagina. This condition can occur due to advanced cancer, radiation therapy, or complex pelvic surgeries such as hysterectomy.
Causes of Gynaecological Fistulas
• Obstetric Fistulas: Often caused by prolonged or obstructed labor, especially in areas with limited access to proper obstetric care. This is a common cause of vesicovaginal fistulas.
• Iatrogenic Fistulas: These are caused by medical interventions such as surgeries, including hysterectomies, cesarean sections, or other pelvic surgeries.Inflammatory or Infectious Conditions: Conditions such as chronic infections, inflammatory bowel disease, or radiation therapy can contribute to the formation of fistulas.
• Trauma: Physical trauma to the pelvic region can also result in the development of gynaecological fistulas.
Symptoms of Gynaecological Fistulas
• Vesicovaginal Fistula: Symptoms include persistent urinary leakage, often accompanied by a foul-smelling vaginal discharge.
• Rectovaginal Fistula: This condition leads to the passage of feces or gas through the vagina, which may be associated with recurrent vaginal infections or discomfort.
• Urethrovaginal Fistula: Symptoms typically involve continuous urinary leakage or difficulty controlling urine flow.
• Ureterovaginal Fistula: This type can cause continuous leakage of urine through the vagina, often related to complications from cancer, surgery, or radiation.
Diagnosis of Gynaecological Fistulas
• Clinical History and Physical Examination: The diagnosis typically begins with a detailed medical history and physical examination.
• Imaging Studies: MRI, CT scans, or ultrasound can be used to visualize the fistula tract and determine its extent.
• Dye Tests: Procedures like cystoscopy or sigmoidoscopy, where a dye is introduced to trace the fistula, may be used for confirmation.
Treatment Options for Gynaecological Fistulas
• Surgical Repair: The primary treatment for gynaecological fistulas involves surgical closure, performed by skilled gynaecological or urological surgeons. This procedure aims to restore normal function and eliminate the abnormal connection.
• Conservative Management: In some cases, non-surgical approaches like bladder or bowel rest and medical management of infections may be attempted, though surgical intervention is typically required for a lasting solution.
• Postoperative Care: Following surgery, patients require close monitoring for complications such as infections, urinary retention, or recurrence of the fistula.
Psychosocial Support: Gynaecological fistulas can have profound psychological and social effects, impacting a person’s sense of intimacy, continence, and overall quality of life. Comprehensive care should include counseling and support services to help patients cope with these challenges.
Gynaecological fistulas are serious medical conditions that demand prompt diagnosis and treatment. Through appropriate surgical interventions and holistic care, including psychosocial support, it is possible to restore normal pelvic function and improve the quality of life for affected individuals.
 Contact Us
Contact UsUrogynaecology
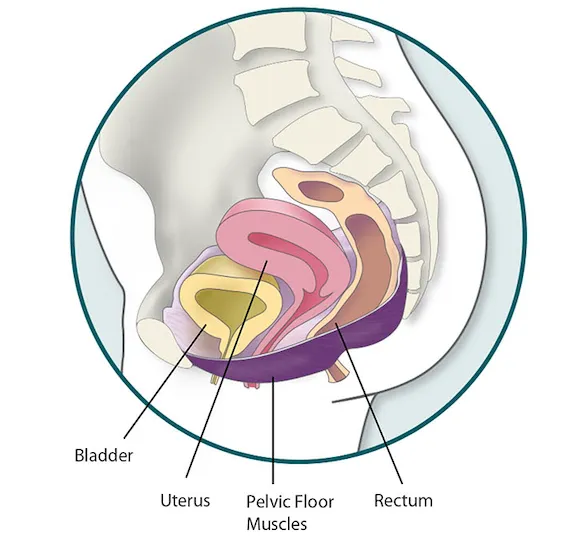
Urogynaecology is a specialized branch of medicine focusing on the diagnosis, treatment, and management of pelvic floor disorders in women. These conditions can significantly impact quality of life and often require a multifaceted approach to care. Below is an overview of key aspects of urogynaecology services:
Pelvic Floor Disorders
Urogynaecology services address a variety of pelvic floor disorders, which include:
• Urinary Incontinence: Involuntary leakage of urine, often affecting women, especially after childbirth or with aging.
• Pelvic Organ Prolapse: A condition where pelvic organs (bladder, uterus, rectum) drop or bulge into the vaginal canal due to weakened pelvic floor muscles.
• Fecal Incontinence: Loss of control over bowel movements, which can also be managed through specialized treatments.
Diagnostic Testing
To accurately diagnose pelvic floor disorders and assess the underlying causes, urogynaecologists use a variety of diagnostic tests:
• Urodynamic Studies: These tests assess how well the bladder and urethra are storing and releasing urine, providing insights into urinary function.
• Cystoscopy: A procedure in which a thin tube with a camera is inserted into the bladder to inspect its interior.
• Imaging: Ultrasound or MRI scans to evaluate the pelvic floor's anatomy and its function during various activities.
Conservative Therapies
For many patients, non-surgical treatment options are effective in managing pelvic floor disorders. These include:
• Pelvic Floor Exercises (Kegel Exercises): Strengthening exercises that help improve control over bladder and bowel functions by targeting pelvic floor muscles.
• Behavioral Modifications: Lifestyle changes such as fluid management, dietary adjustments, and scheduled toileting.
• Medications: Prescription medications that can help manage symptoms, especially in cases of urinary incontinence or overactive bladder.
Surgical Interventions
In more severe cases or when conservative therapies are not effective, surgical options may be necessary:
• Pelvic Organ Prolapse Surgery: Surgical repair to reposition and support prolapsed pelvic organs, often involving mesh implants or other corrective procedures.
• Urinary Incontinence Surgery: Surgical options such as sling procedures or bladder neck suspension to restore bladder function and prevent leakage.
Specialized Procedures
For advanced or specific cases, urogynaecologists may offer specialized treatments such as:
• Sacral Neuromodulation: A treatment for overactive bladder that involves electrical stimulation of nerves controlling bladder function.
• Botox Injections: Used to treat urinary incontinence by relaxing bladder muscles.
• Vaginal Mesh Procedures: A surgical technique for supporting prolapsed pelvic organs and preventing recurrence of prolapse.
Comprehensive Care
Urogynaecology services take a collaborative approach, ensuring that patients receive holistic care. This involves coordination between various specialists:
• Gynaecologists: To address reproductive health concerns alongside pelvic floor issues.
• Urologists: To evaluate and treat urinary disorders in the context of pelvic floor health.
• Physiotherapists: To assist in rehabilitation and the development of pelvic floor strengthening exercises.
• Other Specialists: Working together to create a comprehensive care plan tailored to the patient's needs.
Patient Education and Support
A vital aspect of urogynaecology services is empowering patients with knowledge and resources to manage their conditions:
• Lifestyle Modifications: Guidance on managing symptoms through diet, exercise, and fluid intake.
• Self-Care Strategies: Providing patients with tools to manage their condition at home.
• Ongoing Support: Offering counseling and follow-up care to monitor progress and ensure the patient’s well-being.
Urogynaecology services aim to improve the quality of life for women experiencing pelvic floor disorders by offering a comprehensive range of diagnostic, therapeutic, and support options. These services help address sensitive issues related to urinary, reproductive, and bowel health, providing women with the tools they need to manage and improve their condition effectively.
 Contact Us
Contact UsRobotics

Robotics in gynaecology involves the use of robotic-assisted technology to enhance the precision and effectiveness of surgical procedures related to women's health. This cutting-edge technology offers many benefits and is used to perform a variety of complex and minimally invasive surgeries. Here's a closer look at the role of robotics in gynaecology:
Robotic Surgical Systems
Robotic surgical systems, such as the da Vinci Surgical System, are designed to assist surgeons in performing minimally invasive procedures with greater accuracy and control. These systems feature:
• High-definition 3D Visualization: Offers a magnified, detailed view of the surgical area.
• Wristed Instruments: Mimics the natural movements of the human hand for enhanced dexterity and precision during surgery.
Benefits of Robotic-Assisted Surgery
• Precision: Robotic systems allow for incredibly precise movements, reducing the risk of human error and improving surgical outcomes.
• Minimally Invasive: Smaller incisions lead to reduced blood loss, less postoperative pain, faster recovery, and shorter hospital stays when compared to traditional open surgeries.
• Access to Confined Spaces: Surgeons can access difficult-to-reach areas in the pelvis with greater dexterity and control, making complex surgeries more feasible.
Applications in Gynaecology
Robotic-assisted surgery has a wide range of applications in gynaecology, including:
• Hysterectomy: Often used for the removal of the uterus in cases of fibroids, abnormal bleeding, or cancer.
• Myomectomy: Removal of uterine fibroids while preserving the uterus, particularly for women who wish to retain fertility.
• Endometriosis Surgery: Robotic systems allow for precise excision of endometrial implants with minimal disruption to surrounding tissue.
• Ovarian Cystectomy: Removal of cysts from the ovaries using minimally invasive techniques.
• Pelvic Floor Reconstruction: Utilized in the repair of pelvic organ prolapse, restoring support to the pelvic floor structures.
• Gynecologic Cancer Surgery: Robot-assisted surgery is increasingly used for treating cancers of the uterus, cervix, ovaries, and other gynaecologic malignancies, allowing for better precision and faster recovery.
At Healthy Women, we take pride in being pioneers in the field of robotic surgery. Our surgeons have undergone specialized training to operate robotic systems, ensuring high levels of proficiency and safety since 2011. Our team is dedicated to continuously enhancing its skills to provide the best care using advanced technology.
 Contact Us
Contact UsLaser

Laser technology has become a pivotal tool in gynaecology, offering innovative, minimally invasive solutions for a range of conditions. Here’s an overview of how lasers are transforming gynaecological care:
Treatment of Cervical and Vaginal Lesions
Lasers are widely used to treat abnormal or pre-cancerous cells in the cervix and vagina. This technique offers a precise method of tissue removal, often serving as an alternative to traditional surgical approaches like the loop electrosurgical excision procedure (LEEP). Laser treatment helps reduce bleeding, minimizes scarring, and speeds up recovery.
Vaginal Rejuvenation
Laser therapy has been increasingly used for vaginal rejuvenation. It stimulates collagen production and improves vaginal tone and elasticity, making it particularly beneficial for women experiencing vaginal laxity, dryness, or discomfort after childbirth or menopause. This non-invasive approach can provide a safe and effective way to address these concerns, improving both physical comfort and quality of life.
Treatment of Genital Warts
Laser technology is also an effective treatment for genital warts caused by the human papillomavirus (HPV). By using lasers to destroy the warts, this method offers a precise and minimally invasive option, resulting in less scarring and quicker recovery compared to traditional surgical removal methods.
Management of Endometriosis
During laparoscopic surgery, lasers can be used to excise endometrial tissue implants, offering relief from the pain and symptoms associated with endometriosis. This targeted approach helps improve fertility outcomes and reduces the risk of complications that may arise from more invasive procedures.
Pelvic Floor Disorders
Laser treatments are also used in managing pelvic floor disorders, including conditions like urinary incontinence and pelvic organ prolapse. By promoting tissue regeneration and strengthening pelvic support structures, lasers can help restore pelvic health and improve symptoms, reducing the need for more invasive treatments.
Diagnostic Procedures
Laser technology plays a crucial role in minimally invasive diagnostic procedures, including laparoscopy, hysteroscopy, and colposcopy. The laser provides enhanced visibility, allowing for more precise tissue sampling and clearer imaging, which is essential for accurate diagnosis and treatment planning.
Scar Revision
Laser therapy is highly effective in scar revision, particularly following gynaecological surgeries or trauma. It can help improve the appearance of scars, making them less visible and reducing discomfort. This treatment can significantly enhance cosmetic outcomes and promote faster healing, making it an ideal choice for patients seeking aesthetic improvements after surgery.
At Healthy Women, we offer laser technology to carefully selected patients in need of precise, minimally invasive treatments. The use of lasers not only reduces recovery time but also provides more effective outcomes for conditions ranging from cervical and vaginal lesions to pelvic floor disorders. Our goal is to provide safe, advanced solutions that improve both the physical and emotional well-being of women, with the least amount of disruption to their daily lives.
 Contact Us
Contact UsHysteroscopy

Hysteroscopy is a highly effective, minimally invasive procedure used in gynaecology to both diagnose and treat a range of conditions affecting the uterus. It allows for detailed visualization of the uterine cavity and its lining, enabling precise intervention with minimal discomfort. At Healthy Women, we offer a comprehensive range of hysteroscopic solutions tailored to each patient’s needs.
Diagnostic Hysteroscopy
Procedure: A hysteroscope, a thin, lighted telescope-like instrument, is gently inserted through the vagina and cervix into the uterus. This instrument provides a clear view of the uterine cavity and lining, displayed on a monitor for detailed assessment by the gynaecologist.
Visualization: The hysteroscope allows the doctor to assess the endometrial lining, the uterine cavity, and the openings of the fallopian tubes. This real-time imaging is invaluable for identifying abnormalities that could affect fertility, pregnancy, or overall uterine health.
Indications:
• Abnormal Uterine Bleedin•g: Diagnostic hysteroscopy can help identify causes like polyps, fibroids, or hormonal imbalances contributing to irregular bleeding.
• Recurrent Miscarriages: By evaluating the uterine structure, the procedure can uncover issues such as uterine abnormalities that may contribute to pregnancy loss.
• Infertility: The procedure is crucial for assessing the shape and integrity of the uterine cavity and identifying potential causes of infertility, such as uterine septum or adhesions (e.g., Asherman’s syndrome).
• Abnormal Pap Smear: If a Pap smear shows abnormal cervical results, hysteroscopy allows for further evaluation of potential issues in the endocervical canal.
Diagnostic Findings: During a diagnostic hysteroscopy, tissue samples (biopsies) may be taken to confirm or rule out conditions like endometrial hyperplasia, cancer, or other pathologies.
Operative Hysteroscopy
Procedure: In addition to diagnostic purposes, operative hysteroscopy allows for therapeutic interventions. Using specialized instruments, the gynaecologist can treat conditions within the uterus while the patient is under local or general anaesthesia.
Applications:
• Removal of Polyps: Uterine polyps can be identified and removed with precision, helping to address issues like abnormal bleeding or infertility.
• Fibroid Removal: Small fibroids (benign tumours) can be excised using hysteroscopic techniques, reducing symptoms like heavy periods or pelvic pain.
• Endometrial Ablation: For women with heavy menstrual bleeding, endometrial ablation can be performed to remove or destroy the endometrial lining, significantly reducing bleeding.
• Correction of Uterine Septum: In cases where a uterine septum (a congenital abnormality) is present, hysteroscopy allows for precise resection to improve reproductive outcomes.
Benefits:
• Minimally Invasive: The procedure is performed through small incisions or natural openings, leading to shorter recovery times, reduced risk of infection, and minimal scarring.
• No Need for Large Incisions: Unlike traditional surgeries, hysteroscopy does not require large incisions or extended hospital stays, allowing most patients to return to their normal activities relatively quickly.
Why Choose Hysteroscopy?
• Less Pain: As a minimally invasive procedure, hysteroscopy often involves less pain and discomfort compared to traditional surgery.
• Faster Recovery: Patients typically experience faster recovery times, allowing for a quicker return to daily activities.
• Improved Outcomes: With precision and real-time visualization, hysteroscopy offers the advantage of highly targeted treatment, leading to better outcomes and reduced complication rates.
 Contact Us
Contact UsChronic Pelvic Pain

Chronic pelvic pain (CPP) in women is a complex and multifaceted condition characterized by persistent pain in the lower abdomen or pelvis lasting six months or longer. It can profoundly impact quality of life, physical function, and emotional well-being. Below is an overview of its causes, symptoms, diagnosis, and management.
Causes
CPP can result from a variety of conditions, often requiring a multidisciplinary approach to identify underlying contributors. Common causes include:
1. Gynecological Disorders:
Endometriosis
Pelvic inflammatory disease (PID)
Ovarian cystsUterine fibroids
Adenomyosis
2. Urological Conditions:
Interstitial cystitis/bladder pain syndrome
Urinary tract infections (UTIs)
3. Gastrointestinal Disorders:
Irritable bowel syndrome (IBS)
Inflammatory bowel disease (IBD)
4. Musculoskeletal Problems:
Pelvic floor dysfunction
Myofascial pain syndrome
5. Neurological Conditions:
Nerve entrapment or damage
6. Psychological Factors:
Stress, anxiety, and depression, which can intensify the perception of pain
Symptoms
The hallmark symptom of CPP is persistent pelvic pain, which may present as:
• Constant or intermittent discomfort
• Pain described as sharp, dull, aching, or throbbing
• Accompanying symptoms, such as:
○ Dysmenorrhea (painful periods)
○ Dyspareunia (pain during intercourse)
○ Urinary frequency or urgency
Diagnosis
Diagnosing CPP requires a thorough and methodical evaluation. Key steps include:
1. Medical History and Physical Examination:
• A detailed assessment of symptoms, menstrual history, sexual activity, and previous treatments
• Pelvic examination to identify any abnormalities or tenderness
2. Diagnostic Tests:
• Imaging, such as ultrasound or MRI, to detect structural issues
• Laboratory tests to rule out infections or inflammatory conditions
• Laparoscopy for direct visualization of conditions like endometriosis
3. Multidisciplinary Evaluation:
• Collaboration among gynecologists, urologists, gastroenterologists, and pain specialists ensures a comprehensive assessment
Managing Chronic Pelvic Pain
Effectively managing CPP often involves a multidisciplinary and individualized approach, including:
1. Medications:
• Pain relievers (e.g., NSAIDs, acetaminophen)
• Hormonal therapies (e.g., oral contraceptives, GnRH agonists)
• Neuropathic pain agents (e.g., antidepressants, anticonvulsants)
2. Physical Therapy:
• Specialized pelvic floor therapy to address muscle dysfunction
3. Psychological Support:
• Counseling or cognitive-behavioral therapy (CBT) to manage emotional factors and coping strategies
4. Surgical Interventions:
• Surgery for specific conditions, such as endometriosis or fibroids, when conservative treatments fail
5.Lifestyle Modifications:
• Incorporating stress management, dietary adjustments, and regular physical activity
Chronic pelvic pain in women is a challenging condition requiring a thorough evaluation and personalized care. Early diagnosis and a holistic approach to treatment can significantly improve symptoms and overall quality of life.
At Healthy Women, we specialize in providing comprehensive care and support for those affected by CPP. If you or someone you know is experiencing chronic pelvic pain, seeking medical advice is an essential step toward effective management and relief.
 Contact Us
Contact UsNeurogynecology
Neurogynecology is an innovative medical discipline that focuses on understanding and treating pelvic pain through a neurological lens. By combining principles from neurology and gynecology, this emerging field addresses the complexities of pelvic pain, which often involve musculoskeletal, neurological, and gynecological factors.
Key Aspects of Neurogynecology:
1. Pelvic Pain and the Nervous System
Pelvic pain frequently stems from dysfunctions in the nervous system, such as abnormal sensory processing or nerve damage. Conditions like vulvodynia, interstitial cystitis, endometriosis, and pelvic floor dysfunction often have neurological components that exacerbate pain.
2. Neuroplasticity
Chronic pelvic pain can trigger neuroplasticity—a phenomenon where the nervous system becomes hypersensitive, overreacting to stimuli and making the pain more persistent and challenging to treat.
3. Pain Pathways
Neurogynecology examines the interplay between the central nervous system (CNS) and peripheral nervous system (PNS) in managing or amplifying pain. This includes studying critical pathways, such as the sacral nerves, which innervate the pelvic region.
4. Diagnosis and Management
Advanced diagnostic tools, including neurological imaging (e.g., MRI, PET scans), nerve conduction studies, and nerve block techniques, help identify the neurological roots of pelvic pain. Treatment options may include:
• Neuromodulation therapies, such as TENS and spinal cord stimulators
• Medications targeting nerve painInterventional procedures to address nerve dysfunction
• A multidisciplinary approach incorporating physical therapy, pain management, and psychological support is often integral to effective care.
5. Collaborative Care
Neurogynecology thrives on collaboration between specialists in neurology, gynecology, pain medicine, and urology, recognizing the interconnected nature of pelvic pain across multiple systems.
At HealthyWomen, we specialize in neurogynecology, providing expert care for women experiencing this common yet complex issue. Our team focuses on identifying the root causes of pelvic pain and delivering comprehensive management strategies to alleviate symptoms and improve quality of life.
From tailored medications to advanced interventional procedures, we employ a wide range of approaches to address each patient's unique needs. Neurogynecology is paving the way for more effective, targeted therapies, empowering women to regain control over their health and well-being.
 Contact Us
Contact Us